Osteoarthritis
Osteoarthritis is one of the main conditions that lead to disability and lack of productivity at work. In Australia, osteoarthritis is a highly prevalent and costly condition that affects around 2.2 million people, approximately 1 in 12 Australians.
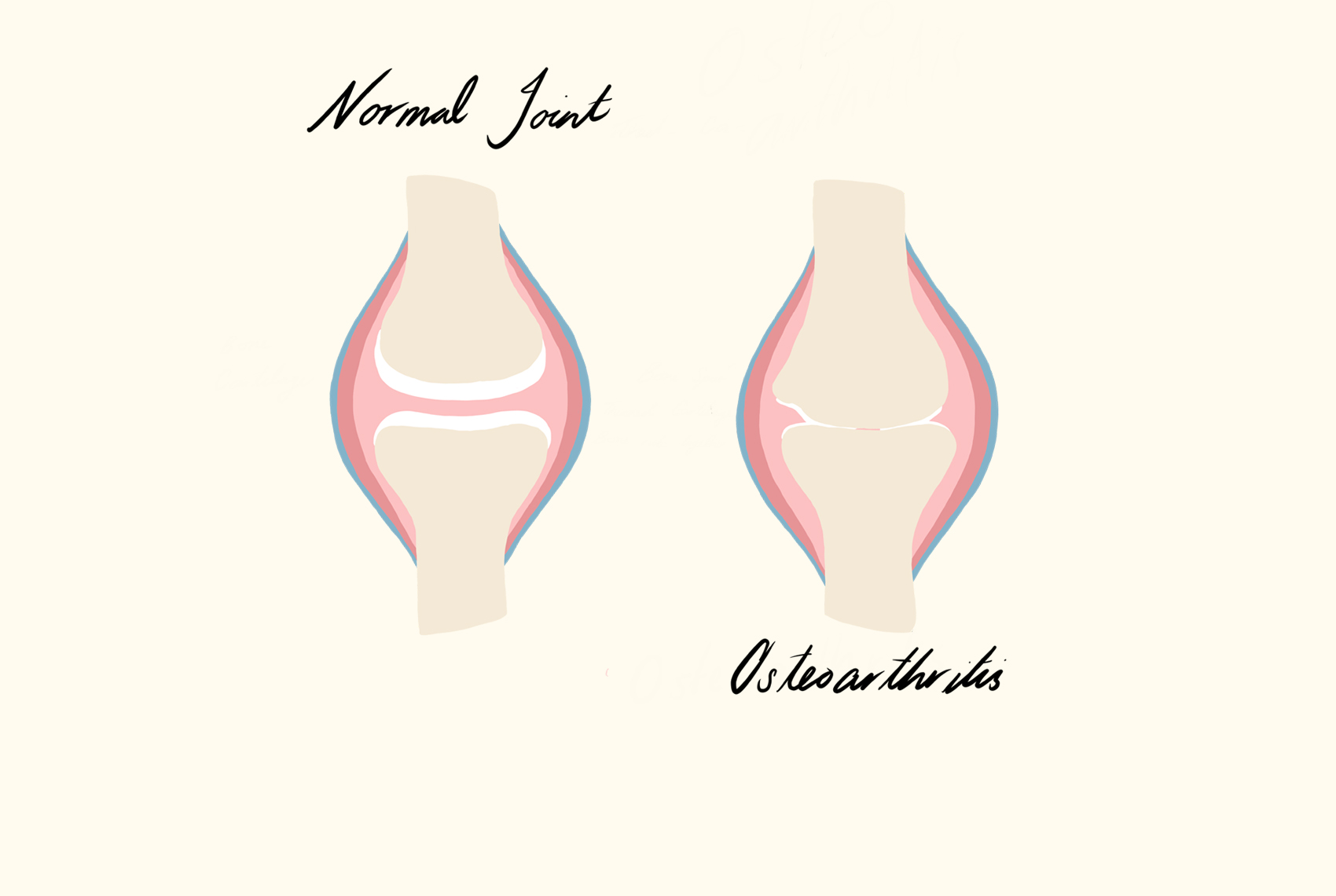
Osteoarthritis is the most common type of arthritis and is sometimes referred to as degenerative joint disease, degenerative arthritis or wear-and-tear arthritis.
What is Osteoarthritis?
This type of arthritis is a long lasting joint condition that effects the cartilage (or the connective tissue) found at the end of bones in the joints. As this cartilage wears down through repeated stress and use, it becomes frayed and rough with the protective space between the bones decreasing. This results in the bones rubbing against each other, causing swelling, stiffness and pain. It makes sense then that osteoarthritis is mostly diagnosed in people over 40 years of age, with less frequent occurrences in young people.
Osteoarthritis Symptoms in the Feet
Osteoarthritis can appear in various joints throughout the body. At Northern Rivers Podiatry we treat osteoarthritis of the foot which has 33 joints. The big toe (the first metatarsophalangeal joint) is most frequently affected; however, it also can impact bones in the mid-foot and ankle.
As the protective cushioning ability from cartilage is compromised, the condition can become more serious and move through stages of quite mild to very severe. When the cartilage deteriorates or is lost, this can impact the joints’ ability to perform a regular range of motions in everyday activities.
It’s important to classify that all people will experience osteoarthritis slightly differently and with varying degrees of intensity. That said, there are many commonalities that most people experience when it comes to osteoarthritis. These tend to include:
- Joint pain (sometimes at night)
- Joint stiffness, especially after inactivity
- Tenderness when touching the joint
- Joint swelling and looking larger than usual
- Difficulty bending or moving the joint
- Cracking noises or a grating sensation when moving the foot or ankle
- Bone spurs
- Changes in joint shape
- Inflamed tissue surrounding the joint
- Feeling unsteady when standing or walking
- An aching feeling after being active or wearing high heels
- Weakening of the surrounding ankle ligaments and muscles, thus exasperating the strain on the cartilage
- Pain when walking or weight bearing
- Compounding intense discomfort from bone and/or cartilage breaking away and floating inside the joint
As briefly mentioned above, bone spurs often form on the edge of bones in the body’s attempt to repair damage from osteoarthritis. These bone spurs are known as osteophytes and will change the joint and range of movement of the impacted joint.
If cannot be highlighted enough, if you are experiencing any of the above symptoms, it is imperative you see a specialist podiatrist who can accurately provide a diagnosis and treatment. Early intervention leads to optimal results. This stated, it is never too late to reduce and treat foot pain caused by osteoarthritis.
How Osteoarthritis Impacts the Foot
When osteoarthritis presents in the foot and ankle joints, it usually effects the joints involving the big toe, midfoot, hind-foot and ankle. Although it may impact any of the 33 bones that make up each foot.
Big Toe
Osteoarthritis of the big toe (hallux rigidus) can be more debilitating than expected as every time you take a step, this joint bears your body weight. Having the degenerative disease in this location can impact your ability to walk without pain.
Midfoot
Tarsometatarsal joints (or mid-foot) are located almost halfway between the ankle and the toes. Arthritis that develops in this area can limit the ability to climb stairs or walk without pain.
Hindfoot / Ankle
The subtalar joint, the talonavicular joint, and the calcaneocuboid joint make up the hind-foot. These joints work together to allow a range of motions, including side-to-side and weight bearing. Osteoarthritis of this hind-foot and ankle area can cause swelling and pain in both the feet and ankles and hinder the ability to walk, stand and jump.
Osteoarthritis Risk Factors
It is vital to understand the risk factors which increase the chances of developing osteoarthritis. Below is a list of the most common factors:
- Injury, overuse or repetitive strain: damages a joint and increases the risk of osteoarthritis in that joint.
- Age: the likelihood of developing osteoarthritis increases with age.
- Gender: women are 3.5 times more likely to be diagnosed than men.
- Obesity or weight gain in general: can put more stress onto the joints. It may also have metabolic effects that increase the risk of osteoarthritis.
- Genetics: People with a family history of osteoarthritis are more at risk of developing the condition.
- Bone deformities: people born with malformed joint or defective cartilage are substantially higher in risk.
- Specific metabolic diseases: Diabetes and hemochromatosis (excessive iron) also increase the likelihood of experiencing osteoarthritis.
- Atypical foot mechanics: high arches or flat arches which cause strain on the surrounding joints.
Osteoarthritis Treatment
Although there is currently no cure for osteoarthritis, a skilled podiatrist can vastly improve your quality of life by expertly managing the symptoms. Management comes in a range of non-invasive methods, as well as surgical treatments of the foot and ankle.
Non-Invasive Treatments for osteoarthritis of the feet and ankle
- Orthotics to support feet (shoe inserts)
- Supportive devices such as crutches or canes
- Pads or arch supports in your shoes
- Education on footwear and activity
- Weight management
- Using a cane or walker to take stress off the affected joint
- Custom made shoes
- A personalised program to strengthen and improve stability of feet (physical therapy)
- Foot and ankle stretches to increase the range of motio
- Anti-inflammatory drugs to help with swelling
- Medications, including over-the-counter pain relievers and prescription drugs
- Steroid injections directly into joints
- Devices for pain reduction (such as TENS machines)
- Increasing or decreasing physical activity – depending on individual’s severity of disease and the patient’s unique presentation.
Surgical Treatments for osteoarthritis of the feet or ankle
There are varying types of surgery that may be appropriate for some patients, depending on the type and severity of arthritis. In most cases surgery is a last resort, there are associated risks involved in having any surgery and there is no guarantee that the patient will have the desired outcome. Types of surgeries include:
- Arthroscopic Surgery: This kind of surgery can potentially treat some symptoms in early stages of arthritis. An arthroscope (a small instrument) is inserted into a joint. The surgeon can view on a monitor from a micro camera to clean the joint area and help to remove any bony spurs using small tools.
- Fusion Surgery: As the name implies, this surgery (also called arthrodesis) involves fusing the bones together with the use of rods, pins, screws, or plates so that the joint remains fused permanently.
- Joint Replacement Surgery: This surgery uses artificial implants to replace the ankle joint and is only used in rare feet and ankle cases.
Specialised Osteoarthritis Treatment from your local Byron Bay Podiatrist
While there is an abundance of information on the internet about osteoarthritis, it’s critical that patients do not self-diagnose. Always seek the expertise of an experienced podiatrist. This is because there are several forms of arthritis that can cause pain in your feet and ankles. The three most common forms are osteoarthritis, rheumatoid arthritis and post-traumatic arthritis. Further to this, any pain akin to arthritis could be symptoms presenting themselves from an entirely different ailment. This is why proper diagnosis and subsequent treatment is key.
At Northern Rivers Podiatry we will walk through your history by asking a series of foundational questions. These clarify important points like:
- When did the pain start?
- Where is the pain located?
- At what times it is most severe?
- What medications are taken on a regular basis?
- Is the pain consistent or intermittent?
- What activities exacerbate the pain?
Once these points are established a physical examination will provide further insight into the specific details unique to each person. The podiatrists in the Northern Rivers clinic will examine shoes (so it’s best to wear a pair that are used regularly). They will also carry out a gait (walking) analysis to observe if the pain and joint stiffness is altering the natural walking style. When the case requires it, we organise x-rays to provide detailed images which can show the narrowing of the joint space between bones indicating cartilage loss. They also reveal any changes in the bone such as fracture or the formation of bone spurs.
Contact Us
"*" indicates required fields









