Diabetes
Diabetes can cause devastating impacts on people’s feet. Lack of sensitivity from nerve damage and compromised blood flow means diabetics need special care to avoid painful infections and foot ulcers. There is absolutely no doubt that prevention really is the best course of action.
What is Diabetes?
The relationship between sugar, glucose and insulin
For a person’s body to work properly, it needs to convert sugar from food into energy. Sugar is not only found in obviously sweet things like cookies and cakes, but in bread, cereals, fruits, vegetables, legumes and dairy products. This sugar is called glucose and a hormone called insulin converts the sugar into energy. The insulin does this by taking the glucose in the bloodstream and converting it to the tissue cells which use it for normal health and physical activity. The insulin is produced by the pancreas which is located behind the stomach.
A person with diabetes will no longer produce insulin at all or in amounts that are insufficient. When this happens there is an unhealthy level of glucose in the blood which can have short-term and longer-term complications.
Types of Diabetes
There are three different types of diabetes:
Type 1 diabetes (approximately 10% – 15% of cases)
is an autoimmune condition. The immune system is activated to destroy the cells in the pancreas which produce insulin. It is not linked to health and lifestyle choices and is one of the most common chronic childhood conditions.
Type 2 diabetes (approximately 85% of cases)
is mostly a progressive condition. The body becomes more and more resistant to the normal effects of insulin and slowly loses its ability to produce enough insulin in the pancreas. It is associated with modifiable lifestyle choices and can be slowed with an increase in physical exercise and healthy eating.
Gestational diabetes
Risks of Diabetes
Diabetes has numerous complications and impacts on the body and will require ongoing monitoring and support. Diabetes can cause blindness, heart disease, kidney disease and all too often amputations. These amputations are mostly caused by diabetes foot ulcers. Every year more than 27,600 people are admitted to hospital due to diabetic foot ulcers and a whopping 4,400 amputations are carried out in a year as a result. This is why podiatrists are an integral part of managing a person’s diabetes.
Diabetic Feet
Diabetes impacts people’s foot health in several major ways. It can cause damage to the nerves, disrupt blood supply to the feet, cause Charcot foot and result in foot ulcers. Diabetic foot nerve damage is called peripheral neuropathy. Poor blood supply and circulation in the feet due to diabetes is called peripheral vascular disease. If left untreated and allowed to manifest, all these conditions can lead to foot amputation.
Peripheral Neuropathy / Nerve Damage
Peripheral neuropathy in the feet is due to high blood glucose levels causing nerve damage. Nerves act as the wiring of the body, carrying messages/feelings from the rest of the body to the brain to register. When the nerves in the feet are damaged, these messages do not get to the brain and thus diabetics experience insensitive or numb feet.
Mostly this damage makes it harder for people with diabetic feet to feel any sensation in their lower limbs. The lack of feeling can have devastating effects because people often do not register when they have injured their foot. Even minor cuts and blisters can result in serious ulcers. In some cases, people with nerve damage will have no symptoms and are therefore unaware of any problems. Those experiencing symptoms of diabetic foot nerve damage often report:
- Numbness in the feet
- Coldness of the legs
- Pins and needles or a tingling sensation in the feet
- Burning pains in the feet and legs, often at night in bed.
Peripheral Vascular Disease / Blood Supply
Diabetes often changes the arteries and blood vessels and can reduce the blood flow to a person’s hands and feet. With insufficient blood supply there can be serious problems with wound healing, cramps and pains in the feet and legs. Most seriously though, cuts and sores may not heal. It’s an important note to add that these circulation problems can be further exacerbated by smoking and high blood fats. Symptoms of poor blood supply include:
- Feet feeling cold
- Feet appearing reddish blue in colour
- Cuts which are slow to heal
- Pain and discomfort in the feet, even when resting
- Leg cramps after walking upstairs or short distances
Charcot Foot / Rocker Bottom Foot
Charcot foot often occurs when the foot and ankle is completely numb (peripheral neuropathy). It is caused when the bones in the feet become weak and susceptible to dislocation and fractures.
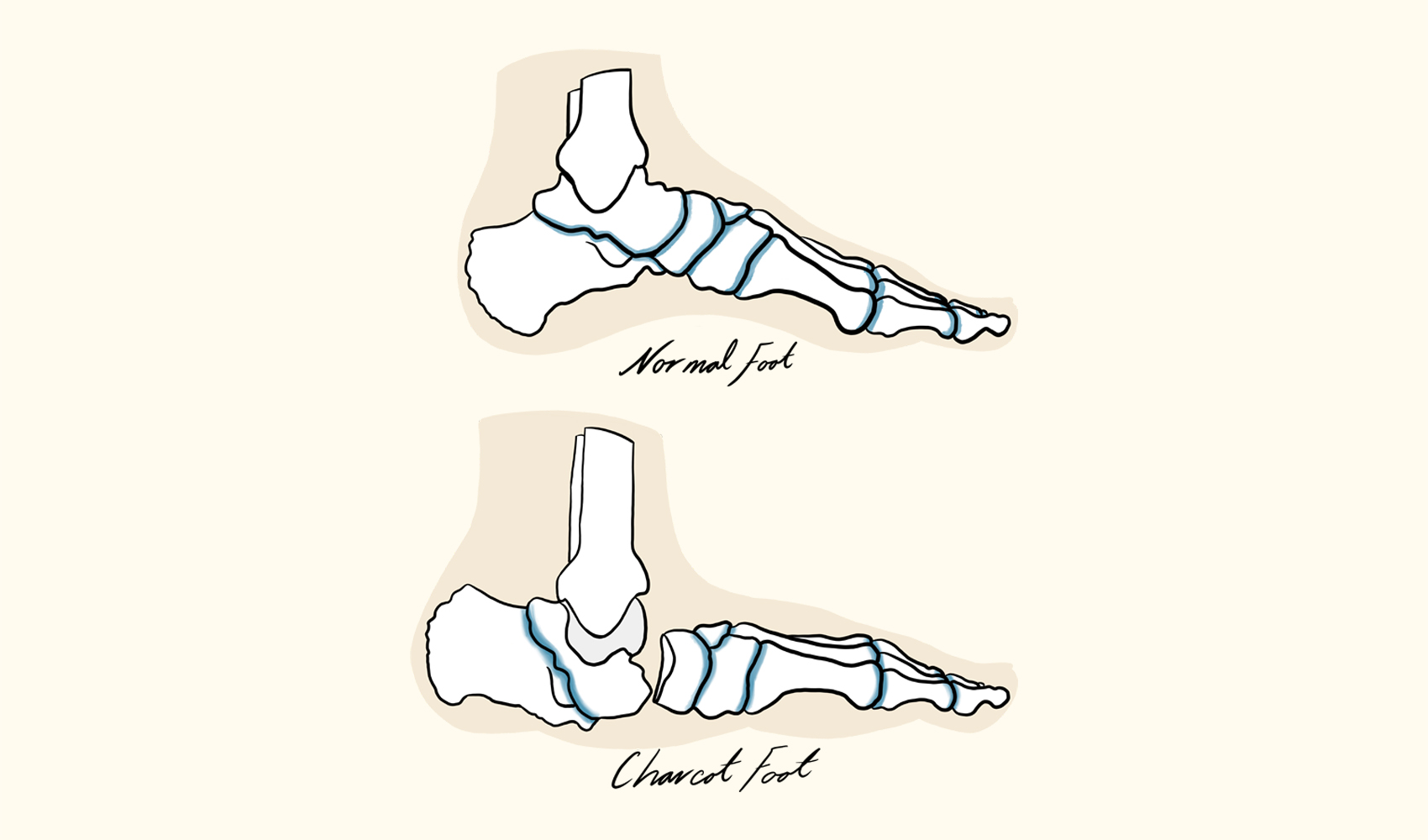
Due to the foot’s numbness, additional damage is done with walking and standing as the person has no awareness of any pain or discomfort. As the condition worsens, the joints in the foot can collapse or dislocate and entirely change the foot’s shape. This deformity creates the rocker bottom appearance.
Diabetic Foot Ulcers
Diabetic foot ulcers are most commonly caused by nerve damage, poor circulation, Charcot foot, high glucose levels and irritated or wounded feet. Foot ulcers are open lesions or sores which do not heal or return over a longer period of time. These lesions can get infected easily with the breakdown of the skin and tissue of the feet.
Foot ulcers vary significantly in severity. Some are small, superficial and do not penetrate the deeper layers of the skin. Other are quite large and can reach tendons, bone and even cause an abscess, osteomyelitis and/or tendonitis. In extreme cases there can even be extensive gangrenous involvement over the entire foot. It will often appear as a large deep circular hole on the underside of the foot where pressure is applied when walking.
All people with diabetes have an increased risk of foot ulcers. At Northern Rivers Podiatry we offer detailed and thorough feet assessment to prevent and treat existing foot ulcers. That said, there are some factors which increase the likelihood of experiencing this debilitating condition:
- Poorly fitted shoes
- Poor hygiene
- Alcohol consumption
- Heart disease
- Obesity
- Smoking
- Kidney disease
- Eye disease from diabetes
- Improperly cut or neglected toenails
Diabetic Foot Amputations
Diabetic foot amputations are in the vast majority preventable with proper monitoring and treatment. Amputations are obviously classified as major surgery and require a long hospital visit, even longer recovery time and irreversible impacts on a person’s independence. On top of this, the cost to the healthcare system is astronomical.
Why are there so many amputations in Australia?
If left unmanaged by healthcare professionals, irreversible damage can quickly present due to the condition reducing a person’s blood supply and causing nerve damage. This means that minor issues can be quickly exacerbated if a diabetic’s wounds heal slowly, and they have no sensitivity/awareness to injuries occurring around their feet.
How can I prevent this happening to me?
The severity of diabetes can gradually worsen over time. Therefore, people who initially felt confident self-managing their foot care can allow standards to drop over time and not notice issues as their foot sensitivity declines, leading to devastating consequences. Getting your feet professionally assessed as part of your responsible foot care is absolutely imperative. Diabetes Australia recommend diabetics have their feet professionally checked at least 1-2 times a year, with this number being on the conservative side. It’s important to recognise that the level of professional support and monitoring needed will vary on each person’s level of risk.
Diabetes Foot Complications Risk Status
No two diabetics are the same. Each person has unique contributing factors to their condition which will give an indication as to whether they are at a low or high risk of experiencing foot complications. Our Byron Bay podiatrists carry out an easy and pain-free assessment to determine each person’s level of risk with subsequent consistent ongoing care and check-ups.
Low Risk Diabetics
As a general overview, individuals who do not smoke, do not drink alcohol (or in small amounts), maintain a healthy weight with healthy eating and engage in regular exercise experience less complications. Low risk indicators also include but are not limited to:
- Daily checking of feet and maintaining a high standard of personal hygiene and care
- Having regular feet sensation
- Having healthy blood flow
High Risk Diabetics
There are various personal factors which can culminate into a high risk of experiencing foot complications. These include but are not limited to:
- Having diabetes for a long time
- Being a regular smoker and/or drinker of alcohol
- Having an inactive lifestyle with a low fitness level
- Unhealthy eating / being overweight or obese
- Having high blood glucose levels for an extended period of time
- Already having foot ulcers or amputations in the past
- Poor feeling in the feet and decreased blood flow
- Inconsistent standard of personal foot hygiene and care
How regularly should you see a podiatrist to check your Diabetic Feet?
All of these factors and much more will give a clear indication of a person’s level of risk of developing more serious foot problems. Once a podiatrist has assessed the level of risk, an ongoing healthcare plan can be organised and maintained. Review the table below to get a sense of how often podiatrist checks may be needed to prevent unnecessary complications through professional management.
Low Risk
Daily Self-Checks
Look for signs of infections, swelling, redness or breaks in the skin
6-12 Monthly Podiatrist Checks
Thorough professional foot assessment and treatment
High Risk
Daily Self-Checks
Look for signs of infections, swelling, redness or breaks in the skin
3-6 Monthly Podiatrist Checks
Thorough professional foot assessment and treatment
Self-Care for Diabetic Feet
Conducting daily self-care routines and self-checks of your feet is incredibly important to carry out in addition to regular check-ups with a podiatrist. Daily self-care should include:
- Washing and thoroughly drying feet, especially between the toes
- Physically reviewing the feet for marks, spots, cuts, swelling and discolouration (this can be done with a mirror if weight / flexibility makes this difficult)
- Get correctly / professionally fitted shoes with enough depth, width and length to avoid rubbing or blisters
- Only wear specific diabetic socks that can offer anti-microbial / moisture wicking / hypo-allergenic properties, seamless design, extra padding and ankle bands which do not cut into the skin
- Always wearing supportive footwear and avoiding being barefoot, even at home
- Reviewing toenails to ensure they are not impacting the surrounding skin and cutting and filing them with great care
- Moisturising the area, focusing on dry sections while avoiding moisturising between the toes
- Feeling the inside of footwear with fingers to check for stones or foreign objects which could cause problems
- Not using over the counter treatments for corns, warts and calluses – always seek professional assistance first
- Regulating a healthy weight range as excess weight places undue pressure on the feet’s skin, tendons, ligaments and bones by exercising for at least 30 minutes a day
- Give up smoking as tobacco can exacerbate circulatory problems
- Limit or cut out alcohol as it often contributes to neuropathy (nerve damage) – this deadens the nerves and increases the likelihood of overlooking a seemingly insignificant injury or cut
- Eating healthy and avoiding sugar-sweetened juices and soft-drinks
- Reducing stress
- Checking foot sensitivity by brushing a feather or other light object over the foot to feel the sensation experienced
Diabetic Footwear
Choosing the correct footwear is one of the most important things a diabetic can do as part of a robust self-care routine. Don’t allow yourself to be rushed into a footwear choice that you are not completely satisfied with. It’s advisable to avoid high heels, open-toed shoes, narrow shoes, flip-flops or walking around barefoot. The best choice of footwear are closed-in joggers/athletic shoes or closed-in leather shoes with a cushioned sole.
For the best care, visit a professional footwear shop that specialises in measuring, assessing and fitting feet properly. Some of these stores are happy for you to purchase a pair of shoes and try them inside at home in a clean environment for an hour or so. This opportunity to wear the shoe for a longer time allows you to properly assess their fit and comfort. If you do suffer from a lack of sensitivity, always closely assess your feet visually afterwards to look for any signs of damage like blisters, redness or pinched skin after wearing new shoes for the first time.
Specialised Diabetic Foot Treatment from your local Byron Bay Podiatrist
Unless people have a pressing physical ailment, they tend to put off preventative health appointments. Unfortunately, this is the leading reason why so many people have one or both feet amputated when it was entirely preventable. Having regular check-ups with an experienced podiatrist is integral to diabetic foot care.
At Northern Rivers Podiatry we will assess the skin for dryness, calluses, corns, cracks, cuts, bruising, swelling, discolouration and infections. We will review the blood flow to the feet, assess nerve sensitivity and check biomechanical risk factors. We will also review the condition of the toenails, provide nail care and review the overall foot shape.
After a comprehensive assessment we can offer a wide range of options to support your ongoing foot care. We can recommend the best quality options for footwear, foot braces, socks, shoe inserts, compression wraps and even casts.
If you haven’t been engaging in regular check-ups, it’s highly recommended to seek professional support as soon as you notice:
- Unusual swelling
- Cuts
- Ulcers
- Redness / discolouration
- Ingrown and fungal toenails
- Calluses
- Corns
- Bruising
- Cracked skin
- Bunions
- Plantar warts
- Hammertoes
- Heel pain or heel spurs
- Changing colour to the nails
- Skin colour changes
- Increase in skin temperature
- Blisters
- Pus discharge
- Splinters
- Consistently cold feet to touch
At Northern Rivers Podiatry we are all about arming our patients with the best information, providing state of the art diagnostic methods and offering world-class treatment and support. Through this we prevent unnecessary and debilitating conditions like Charcot foot and foot ulcers while treating pre-existing conditions with the best possible care. So, if you’re ready to take your diabetic footcare into your own hands with some professional medical support, book a consultation with us as a first proactive step.
Contact Us
"*" indicates required fields









